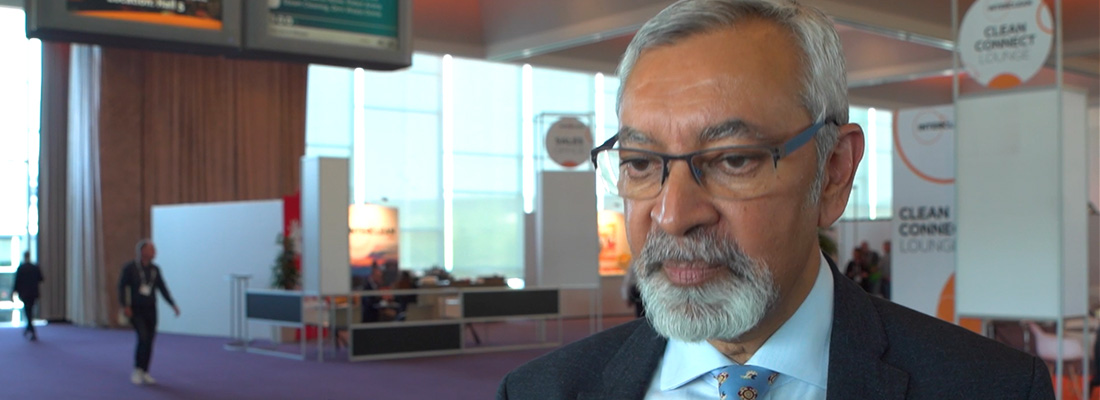
Infection prevention: control & calculation | Dr. Ian Hosein
The existence of dry surface biofilms in hospitals (or any environment, for that matter) is a given, but that doesn’t mean we’re doomed. Reassuringly, Dr. Ian K. Hosein, Consultant Medical Microbiologist at Kings College Hospital in London, explains: “With pragmatic cleaning protocols that include a feedback loop to assure hygiene, we can minimize the possibility that patients will become infected via environmental surface biofilms.”
First things first. What exactly is a biofilm? Hosein: “Biofilm refers to a group of organisms, such as bacteria, clustered together. One important characteristic that distinguishes a biofilm from randomly finding living organisms somewhere, is the cooperation between the different types of organisms within a biofilm. For example, the products of one organism can change the local environment within the biofilm and in that way stimulate growth of another organism. Another important aspect is the fact that a biofilm provides a form of protection. This makes the organisms in a biofilm more resistant to changes in their external environment, such as attempts at cleaning.”
Even if you can’t see it, it’s there
Another aspect to keep in mind is that biofilms are not always visible to the naked eye. “If you’re in charge of cleaning in a hospital and you see something dirty, you’ll know that it needs to be cleaned. And so you’ll clean it to a point where you can no longer see the dirt”, Hosein explains. “But if it’s a dry surface biofilm, you’ve probably only made it smaller instead of removing it completely. Partly because you could not see it in the first place, and also because of its protective traits I just discussed. So even though you can’t see it anymore, it’s still there.” You’re probably wondering: if we can’t see it, how do you know it’s there? Because research has shown it. Hosein: “Imagine a patient who was infected with a multi-resistant bacterium. When the patient is discharged from the hospital, he or she vacates the room, and then the room undergoes intensive cleaning commonly referred to as ‘terminal cleaning’. This is designed to remove environmental contamination from the organism concerned, so as not to put the next room occupant at risk. Now, we have conclusive data proving that the next patient who comes into that room may still acquire that same multi-resistant bacterium as the previous patient. Even when those patients didn’t meet each other. The only thing they have in common is that hospital room. And, environmental sampling of the ‘terminally cleaned’ can detect the organism in question. The existence of dry surface biofilm with its associated properties gives a way of understanding the environmental persistence despite attempts at cleaning.”
Getting infected from a hospital room
He explains how this is possible: “It’s completely normal that the infected patient sheds some of the bacteria into the room. That just happens. These bacteria fall to the floor or get onto the bedside table and form a biofilm. Then when the patient leaves, the cleaners come in and clean the room until it looks clean. But they didn’t kill the living parts of the biofilm, because they couldn’t see it and did not know it was there. So there is nothing that tells them that they haven’t cleaned a surface properly. When the next patient comes in and touches the contaminated bedside table, he or she acquires the same multi-resistant bacterium.”
Does it have consequences for patient safety?
Some scientists warn that biofilms are everywhere and that because of that, we’re all in serious trouble. “But that is nonsense”, Hosein says passionately. “Firstly, the language they use is often emotionally charged. But more importantly, a hospital or any other healthcare environment is never sterile. That is not possible so we shouldn’t wish for that. How can it be, when we have visitors and staff walking around and patients are being admitted 24 hours a day? What we need is pragmatism. Let’s say that there’s a dry biofilm on the hospital floor. The question is: does that matter? How likely are healthcare workers or patients to touch the floor? Because if they don’t touch that floor, then what is the problem? What is the risk to a patient from a thin biofilm on the floor in a hallway of a busy hospital? Why worry about this when we should focus on parts of the environment that really do matter?”
Process control and probability management
He continues: “Our main goal is for the patients to not get infected. That is what it’s all about. And for somebody to get infected from an environmental source, several events must happen. Firstly, the environment must be contaminated. And it must stay contaminated even after the cleaners have done their jobs. Secondly, the patient needs to get in contact with the contaminated environment. But if they’re bedbound, they can’t touch the environment. Therefore, the organism must come to them. For instance, through a member of staff who touches the contaminated environment before they touch the patient. We can control all those different steps and minimize the probability of making a patient ill. For instance, the healthcare workers must perform hand hygiene before touching the patient. So, you can see how favorable probabilities can be built into the overall approach to patient protection by focused environmental cleaning using protocols established as ‘more effective’ and then reducing the probability of transmission stepwise by say the donning of personal protection equipment and hand hygiene. I use the term ‘more effective’ since nothing is perfect in process controls but we can reduce the threat level so low as to be negligible.”
To summarize, Hosein says: “It’s all about process controls and managing probabilities. A sterile hospital is not possible, so we must accept that the environment gets contaminated and that it contains biofilms. But not every contamination poses a threat to the patients. We need to find a balance where we protect the patients by focusing on things that can get them infected. For that, we need cost-effective, pragmatic protocols that minimize the probability that patients get infected. And those protocols should be based on proper research and data to assure the level of hygiene or cleanliness. Because in the end, human lives are at stake.”
Share your stories with us!
Do you have an innovation or interesting news you would like to share with the professional cleaning and hygiene industry? The Interclean website and social media channels are a great platform to showcase your stories!
Please contact our press department interclean@rai.nl.
Are you an Interclean exhibitor?
Make sure you add your latest press releases to your Company Profile in the Exhibitor Portal for free exposure.
Receive the best newsletter on cleaning & hygiene - straight to your inbox!
We promise never to send you spam and you can unsubscribe at any time!